EN/TH
HoLEP, or Holmium Laser Enucleation of the Prostate was developed in New Zealand in the late 1990’s. It is normally done under general anaesthetic. The prostate is approached internally (endoscopically), through the urethra, without any cuts on the skin. The Holmium laser is used to peel out the obstructive core of the prostate in its entirety. This leads to maximal relief of prostate obstruction and a man will usually only require 1 HoLEP procedure in his lifetime. It is very unlikely that the prostate will regrow after HoLEP (0.7% need a re-operation up to 10yr after HoLEP compared to 10-15% after TURP, and more after green light laser surgery).
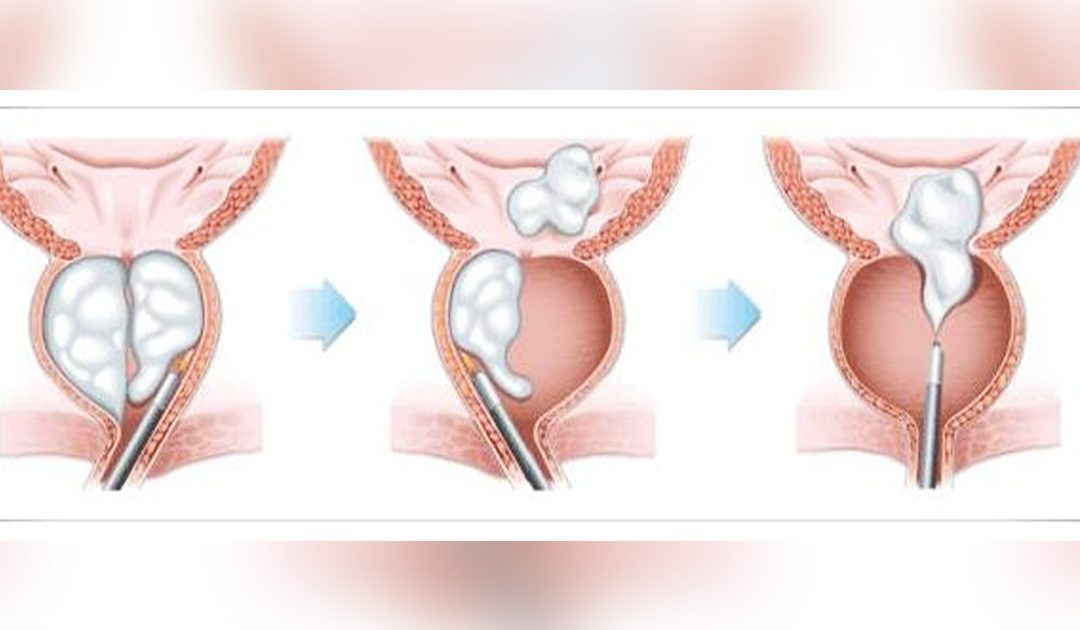
Diagram showing the complete removal of the obstructive inner part of the prostate that is achieved with HoLEP
After HoLEP, the area of the prostate that is removed is sent for microscopic analysis. Cancer that would otherwise be undetected is found in 8%.
HoLEP is one of the most extensively researched procedures for BPH. 16 HoLEP randomised trials (the highest quality of clinical trial) have been published up to Dec 2014. The clinical trials comparing it to the previous “gold standard” of TURP, consistently show advantages for HoLEP that include: Less bleeding, fewer blood transfusions, shorter time with a catheter in place after surgery, and shorter hospital stay (90% of men having HoLEP are able to leave the hospital without a catheter the day after surgery, and in some cases there is no need to stay in hospital overnight). Meta-analyses which are studies analysing the results of large numbers of randomised trials, suggest that HoLEP relieves urinary symptoms and improves urinary flow rates more effectively than all other endoscopic procedures for BPH. The average symptom score improvement after HoLEP is 70-80% and flow rate improvements of up to 600% have been reported. Recent studies have shown that HoLEP is extremely effective at treating men in urinary retention. 98% of men with catheters before surgery are freed from their catheter dependence after HoLEP. This compares to 70% with green light laser and TURP surgery. Unlike all other endoscopic procedures for BPH, HoLEP is suitable for men with any size prostate.
WHO IS SUITABLE FOR HOLEP?
- Those experiencing moderate to severe symptoms of enlarged prostate (BPH)
- Weak stream of urine
- Incomplete emptying of the bladder
- Stop and start when urinating
- Straining to begin urination
- An increased need to urinate
- Interrupted sleep because of the need to urinate
- Complications of enlarged prostate
- Those who want an alternative option to TURP for management of their BPH
- Those who have enlarged prostate symptoms and have failed minimally-invasive treatment options
- Those whose prostate anatomy is not appropriate for other treatment options
- Those who have failed medical therapy, don’t want to take medication or have had side effects
- Those who want to improve their quality of life to what it was before BPH symptoms
WHAT ARE THE ADVANTAGES OF HOLEP?
HoLEP is a definitive surgical treatment for enlarged prostate (BPH) for the relief of bothersome urinary symptoms:
- Very effective treatment option, even for very large prostates
- Durable improvement in urinary symptoms with low revision rates
- Quick recovery with minimal bleeding and recovery time after surgery
- Eliminates the need for lifelong use of medications
HOW IS HOLEP PERFORMED?
- This procedure is performed under general (or spinal) anaesthesia
- It involves the use of a small telescope (cystoscopy) and a high powered holmium laser
- The enlarged obstructing lobes of the prostate are ‘shelled out’ (enucleated) and then removed, creating an open prostatic urethra
- It can take anywhere from 20 minutes up to four hours depending on the size of the prostate
- Most patients can be discharged 1-2 days following surgery
WHAT TO EXPECT AFTER HOLEP?
- Most of the recovery is done at home and in most cases ‘light’ normal activities can be resumed as soon as 3-5 days post procedure
- Complete recovery can take up to 4 weeks during which time strenuous activity should be avoided
- The most common side effects include discomfort or burning with urination, blood in the urine, urgent need to urinate and/or difficulty controlling this urge. Most of these symptoms generally subside within the first two weeks following procedure
HOLEP OUTCOMES
- Most patients will notice an immediate improvement in their urinary flow, pressure and bladder emptying
- Bladder symptoms of urinary frequency, urgency and nocturia (getting up at night to pass urine) tend to take longer (up to 3 months) to improve
POST-OPERATIVE CARE INSTRUCTIONS
What to expect:
- When you wake, you will have a catheter in place, which will assist your bladder in expelling any residual blood from the procedure.
- Improved urinary flow, pressure, and bladder emptying following the removal of the catheter.
- Blood in the urine is common for a couple of weeks following your procedure, but in some cases it may take longer to resolve. This may be intermittent.
- Burning and stinging with urination may last for 2-3 weeks following the procedure. This does not usually indicate infection.
- Urination frequency and urgency (urinating often and in a hurry) as well as nocturia (waking at night to urinate) take longer to improve, and in most patients will settle within 3 months. In some circumstances symptoms may persist.
- Some patients may experience transient incontinence (leakage of urine) following the procedure. This usually resolves within three months with pelvic floor muscle exercises.
- Retrograde (dry) ejaculation is common (90%), expected, and if it occurs it is permanent. This is not dangerous.
Return to activity:
- Driving – no driving for at least 24 hours, or until you are comfortable to do so
- Work – you will require at least 4-5 days off work, possibly longer depending on your occupation
- Lifting – avoid heavy lifting for 2 weeks following your procedure
- Activities – walking is fine and encouraged following your procedure, however you should avoid strenuous activity and straining to open your bowels for 2 weeks following your procedure
- Sex – avoid for 2 weeks following the procedure.